NHS England have recently published several important papers setting out the things they expect every local healthcare trust to do over the next two years, and how they are going to support these ambitions. In this blog, Andrew Brown (@andrewbrown365), a consultant to the Making Every Adult Matter coalition on substance misuse issues, provides some background.
In recent years, NHS England has been engaged in a major exercise to identify how it can meet growing patient needs in the context of limited resources. This involved the development of the Five Year Forward View for Mental Health, produced by a Mental Health Task Force led by Mind’s chief executive Paul Farmer.
Building on this, work is now underway to develop Sustainability and Transformation Plans (STPs) across the NHS in England. These divide the country into 44 areas, each of which must develop a five-year plan covering all NHS spending; the King’s Fund has produced a helpful summary of the process. The road from here is complex, but there are early indications of some positive developments for people experiencing multiple needs, who often fail to receive the physical and mental health care they require.
For organisations commissioning and delivering services in the community there is an opportunity to engage with the NHS on its strategic and operational priorities and to improve outcomes for people with multiple needs.
Those developing STPs have been asked to consult widely on the priorities for their areas, but how far this has been practically happening isn’t clear, and the plans are now at a point where it may be difficult to influence. Nevertheless, we think that making contact with your local Clinical Commissioning Group and NHS providers could be of significant benefit.
To influence the process effectively, it’s helpful to consider the context against which the STPs are being drawn up. In the rest of this blog, I’ll outline some key developments that you should bear in mind.
NHS Operational Planning and Contracting Guidance 2017-19
A piece of guidance published in September 2016 sets out the ‘must dos’ for the NHS in England over the next two years, and includes things of significance for people with multiple needs and the services that support them. In particular, the section on supporting the Five Year Forward View for Mental Health requires the NHS to:
- Expand capacity so that more than 53% of people experiencing a first episode of psychosis begin treatment with a NICE-recommended package of care within two weeks of referral;
- Increase access to individual placement support for people with severe mental illness in secondary care services by 25% by April 2019 against 2017/18 baseline; and
- Reduce suicide rates by 10% against the 2016/17 baseline.
An analysis of Clinical Commissioning Groups’ budgets by the Kings Fund shows that 40 per cent of mental health trusts have seen reductions to their income in 2015/16. Recent Freedom of Information requests by the Labour MP Luciana Berger suggest that over half (57%) of Clinical Commissioning Groups plan to reduce the proportion of their budget they spend on mental health this year (2016/17).
The new guidance says that NHS trusts must increase baseline spend on mental health to deliver the Mental Health Investment Standard, and to deliver this there will be dedicated funding including centrally-held transformation funding of £215m in 2017/18 and £180m in 2018/19.
Death by suicide
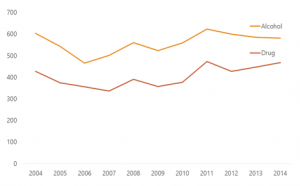
Meeting the welcome ambition to reduce suicide rates is unlikely without a focus on multiple needs. The recent annual report from the National Confidential Inquiry on Suicide and Homicide looked at patients who died through suicide and had recently been in contact with mental health services. Over half (54%) had a history of alcohol or drug misuse, an average of 672 deaths per year; of these just 11% were receiving drug or alcohol treatment.
A key clinical message from the confidential inquiry team is:
“Specialist alcohol and drug services should be available, with the ability to manage clinical risk, working closely with mental health services, with agreed arrangements for “dual diagnosis” patients.”
Commissioning for Quality and Innovation (CQUIN) payments framework
A second document that tells us something about how particular ambitions will be incentivised by NHS England is this draft technical guidance on the national Commissioning for Quality and Innovation (CQUIN) payments framework for 2017-19.
There are 13 national CQUIN indicators set out in the guidance, and the following might have potential to benefit people with multiple needs:
- Supporting Proactive and Safe Discharge
- Improving services for people with mental health needs who present to A&E.
- Preventing ill health by risky behaviours – alcohol and tobacco
- Improving physical healthcare to reduce premature mortality in people with Severe Mental Illness
- Improving the assessment of wounds
- A reduction in the proportion of ambulance 999 calls that result in transportation to a type 1 or type 2 A&E Department
The annex gives details of the ways that payments will be weighted, and the rationale for including them in the national programme.
Improving services for people with mental health needs who present at A&E
The details of the CQUIN dealing with improving services for people with mental health needs who present at Accident and Emergency departments is of particular interest. In setting out the rationale for this CQUIN NHS England say:
“People with mental ill health are 3 times more likely to present to ED [Emergency Departments] than the general population. More than 1 million presentations are currently recorded as being directly related to mental ill health. People with known mental ill health are 5 times more likely to be admitted to acute hospitals and 80% of these emergency admissions are recorded as being primarily for physical health reasons.”
They note the issues of co-existing mental health and substance use conditions, and specifically state that people in this situation may require “further interventions from mental health, primary, community and social care, alcohol and substance misuse and voluntary sector services”.
The guidance sets out that in year one of the programme, emergency departments will identify the top 0.25% of people attending A&E most frequently (an average of 150-200 individuals per NHS Trust) and take a number of steps to improve the care they receive. These include developing joint care plans and strengthening services to meet their needs, with the ultimate aim of reducing admissions among this group by 20%. The second year will see the expectation of better care for this group extended to all patients with mental health needs attending A&E, with a target of reducing admissions by 20%.
Improving physical healthcare to reduce premature mortality in people with Severe Mental Illness
Although many people with multiple needs don’t have severe mental illness (SMI) – which include psychosis, bipolar disorders, and severe depression – these conditions are more prevalent in this group than in the general population.
The CQUIN which incentivises reducing premature death in people with SMI recognises that many of those premature deaths could be delayed by helping this group to address their use of drugs, alcohol and in particular tobacco.
Next steps
Given the longstanding concerns about the ability of people with multiple needs to access appropriate health care, particularly mental health care, these are welcome steps in the right direction. Nevertheless, it would be naïve not to recognise the tough operating environment that accompany these NHS reforms and ambitions, and how they will require imagination, commitment and the willingness to work together to be achieved.
However, we believe there are clear opportunities for organisations outside the healthcare system to engage with this process, and the MEAM partners would be interested to hear from areas about their experiences.
For further information, contact Andrew.Brown@mind.org.uk.
Useful resources
- A crowd-sourced collection of STPs published to date (Google Drive)
- Data on coexisting mental health and substance misuse issues by local authority from Public Health England.
- Suicide prevention: developing a local action plan – guidance from PHE
- Comorbidity of substance use and mental disorders in Europe (EMCDDA)
- Psychosis with substance misuse in over 14s: assessment and management (NICE)
- The Leeds Co-occurring Mental Health and Substance use (Dual Diagnosis) Capability Framework
- A Guide for the Management of Dual Diagnosis for Prisons (DH)
Keep an eye out for further guidance from PHE and the NHS on co-existing conditions, and from NICE on the same topic.
